Autoimmune Disorders
- Joan Rothchild Hardin

- Mar 9, 2014
- 4 min read
Updated: Jun 16, 2021

Autoimmune disorders are conditions that occur when the immune system mistakenly attacks and destroys healthy body tissue. 80-100 such disorders have been identified, with many more suspected of fitting into the category.
The American Autoimmune Related Diseases, Inc, (AARDA) claims 50 million Americans have an autoimmune disease. They publish this list of about 80 autoimmune and autoimmune related diseases:

Acute Disseminated Encephalomyelitis (ADEM)
Acute necrotizing hemorrhagic leukoencephalitis
Addison’s disease
Agammaglobulinemia
Alopecia areata
Amyloidosis
Ankylosing spondylitis
Anti-GBM/Anti-TBM nephritis
Antiphospholipid syndrome (APS)
Autoimmune angioedema
Autoimmune aplastic anemia
Autoimmune dysautonomia
Autoimmune hepatitis
Autoimmune hyperlipidemia
Autoimmune immunodeficiency
Autoimmune inner ear disease (AIED)
Autoimmune myocarditis
Autoimmune oophoritis
Autoimmune pancreatitis
Autoimmune retinopathy
Autoimmune thrombocytopenic purpura (ATP)
Autoimmune thyroid disease
Autoimmune urticaria
Axonal & neuronal neuropathies
Balo disease
Behcet’s disease
Bullous pemphigoid
Cardiomyopathy
Castleman disease
Celiac disease
Chagas disease
Chronic fatigue syndrome**
Chronic inflammatory demyelinating polyneuropathy (CIDP)
Chronic recurrent multifocal ostomyelitis (CRMO)
Churg-Strauss syndrome
Cicatricial pemphigoid/benign mucosal pemphigoid
Crohn’s disease
Cogans syndrome
Cold agglutinin disease
Congenital heart block
Coxsackie myocarditis
CREST disease
Essential mixed cryoglobulinemia
Demyelinating neuropathies
Dermatitis herpetiformis
Dermatomyositis
Devic’s disease (neuromyelitis optica)
Discoid lupus
Dressler’s syndrome
Endometriosis
Eosinophilic esophagitis
Eosinophilic fasciitis
Erythema nodosum
Experimental allergic encephalomyelitis
Evans syndrome
Fibromyalgia**
Fibrosing alveolitis
Giant cell arteritis (temporal arteritis)
Giant cell myocarditis
Glomerulonephritis
Goodpasture’s syndrome
Granulomatosis with Polyangiitis (GPA) (formerly called Wegener’s Granulomatosis)
Graves’ disease
Guillain-Barre syndrome
Hashimoto’s encephalitis
Hashimoto’s thyroiditis
Hemolytic anemia
Henoch-Schonlein purpura
Herpes gestationis
Hypogammaglobulinemia
Idiopathic thrombocytopenic purpura (ITP)
IgA nephropathy
IgG4-related sclerosing disease
Immunoregulatory lipoproteins
Inclusion body myositis
Interstitial cystitis
Juvenile arthritis
Juvenile diabetes (Type 1 diabetes)
Juvenile myositis
Kawasaki syndrome
Lambert-Eaton syndrome
Leukocytoclastic vasculitis
Lichen planus
Lichen sclerosus
Ligneous conjunctivitis
Linear IgA disease (LAD)
Lupus (SLE)
Lyme disease, chronic
Meniere’s disease
Microscopic polyangiitis
Mixed connective tissue disease (MCTD)
Mooren’s ulcer
Mucha-Habermann disease
Multiple sclerosis
Myasthenia gravis
Myositis
Narcolepsy
Neuromyelitis optica (Devic’s)
Neutropenia
Ocular cicatricial pemphigoid
Optic neuritis
Palindromic rheumatism
PANDAS (Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcus)
Paraneoplastic cerebellar degeneration
Paroxysmal nocturnal hemoglobinuria (PNH)
Parry Romberg syndrome
Parsonnage-Turner syndrome
Pars planitis (peripheral uveitis)
Pemphigus
Peripheral neuropathy
Perivenous encephalomyelitis
Pernicious anemia
POEMS syndrome
Polyarteritis nodosa
Type I, II, & III autoimmune polyglandular syndromes
Polymyalgia rheumatica
Polymyositis
Postmyocardial infarction syndrome
Postpericardiotomy syndrome
Progesterone dermatitis
Primary biliary cirrhosis
Primary sclerosing cholangitis
Psoriasis
Psoriatic arthritis
Idiopathic pulmonary fibrosis
Pyoderma gangrenosum
Pure red cell aplasia
Raynauds phenomenon
Reactive Arthritis
Reflex sympathetic dystrophy
Reiter’s syndrome
Relapsing polychondritis
Restless legs syndrome
Retroperitoneal fibrosis
Rheumatic fever
Rheumatoid arthritis
Sarcoidosis
Schmidt syndrome
Scleritis
Scleroderma
Sjogren’s syndrome
Sperm & testicular autoimmunity
Stiff person syndrome
Subacute bacterial endocarditis (SBE)
Susac’s syndrome
Sympathetic ophthalmia
Takayasu’s arteritis
Temporal arteritis/Giant cell arteritis
Thrombocytopenic purpura (TTP)
Tolosa-Hunt syndrome
Transverse myelitis
Type 1 diabetes
Ulcerative colitis
Undifferentiated connective tissue disease (UCTD)
Uveitis
Vasculitis
Vesiculobullous dermatosis
Vitiligo
Wegener’s granulomatosis (now termed Granulomatosis with Polyangiitis (GPA)
** “NOTE Fibromyalgia and Chronic Fatigue are listed, not because they are autoimmune, but because many persons who suffer from them have associated autoimmune disease(s).”

Another list of autoimmune diseases – with descriptions of each, a useful glossary and links to other reputable sites for each disease – is published by AutoimmuneDiseaseList.com. It includes about 100 such diseases along with another 40 that are suspected of having autoimmune components.

In an article called The Common Thread on the AARDA website, Noel R. Rose, MD, PhD, describes autoimmunity and autoimmune diseases in this useful way:
… there are some circumstances where the immune response attacks the body of the host itself. The host may be an animal or it may be a human patient. That is what we call autoimmunity. Autoimmunity is nothing more than the immune response directed to the body of the patient himself or herself.
Let me define a second term for you, autoimmune disease. These two terms do not mean exactly the same thing, and the difference may be important to us as we talk about some of these issues a little later this afternoon. Autoimmune disease is a disorder that occurs because of autoimmunity–a disease that is caused by an immune response to the body of the patient himself or herself.
Now, in defining autoimmune disease that way, I imply that there is autoimmunity without autoimmune disease. In fact, we now know that autoimmunity is not at all uncommon and that it exists in all of us. Every one of us has some degree of autoimmunity naturally, and it does not seem to do us any harm.
Dr Rosen is Chairman Emeritus, AARDA National Scientific Advisory Board; Professor of Pathology and of Molecular Microbiology and Immunology; Director, Center for Autoimmune Disease Research, Bloomberg School of Public Health, The Johns Hopkins University, Baltimore, MD.
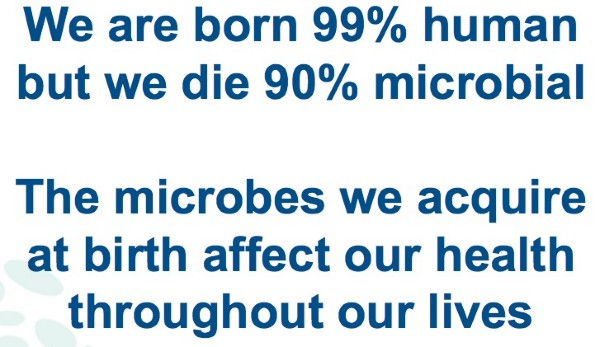
I question Dr Rosen’s conclusion that the degree of autoimmunity we each have in us does “not seem to do us any harm”. There is abundant evidence that an impoverished gut microbiota leads to many types of diseases and conditions – including autoimmune disorders.

Worldwide prevalence of asthma; from ‘Global Burden of Asthma,’ 2004
The 2004 map above showing the world wide prevalence of asthma, one of the autoimmune disorders, presents a graphic illustration of the Hygiene Hypothesis at work. This hypothesis, sometimes called the Sanitation Hypothesis, posits that a lack of early childhood exposure to infectious agents, symbiotic microorganisms such as good gut flora or probiotics, and parasites increases susceptibility to allergic diseases by suppressing the natural development of the immune system. In particular, the lack of exposure is thought to lead to defects in the establishment of immune tolerance. (Wikipedia, 12/26/2013)
According to the Hygiene Hypothesis, increased levels of cleanliness and decreasing incidence of infections in western countries – and more recently in developing countries – is the source of the increasing incidence of both autoimmune and allergic diseases. Migration studies show that people who migrate from a low-incidence to a high-incidence country develop immune disorders even in first generation immigrants. Researchers attribute these change, at least in part, to changes in the gut microbiota caused by life-style changes, including diet. (Okada, 2010)
It is also well known that breast milk is loaded with antibodies and other protective factors that provide the newborn with an immunological umbrella. Infants who aren’t breastfed or whose nursing was prematurely discontinued are more likely to develop autoimmune disorders later in life. (Jackson & Nazar, 2006).
REFERENCES
Jackson, K.M. & Nazar, A.M. (2006). Breastfeeding, the immune response, and long term health. Journal of the American Osteopathic Association, 106:4, 203-7.
Okada, H. et al. (2010). The ‘hygiene hypothesis’ for autoimmune and allergic diseases: an update. Clinical & Experimental Immunology: The Journal of Translational Immunology, 160:1, 1–9.
Wikipedia. (12/26/2013). Hygiene Hypothesis. See http://en.wikipedia.org/wiki/Hygiene_hypothesis
© Copyright 2013-2014 Joan Rothchild Hardin. All Rights Reserved.
DISCLAIMER: Nothing on this site or blog is intended to provide medical advice, diagnosis or treatment.


Comments